Clinical significance of peripheral blood minimal residual disease detection at the eighth day of induction therapy in children with B-cell acute lymphoblastic leukemia
-
摘要:目的
基于TARGET数据库分析诱导治疗第8天外周血微小残留病(MRD)检测在急性B淋巴细胞白血病(B-ALL)患儿预后评估中的临床意义。
方法下载TARGET数据库中2000—2010年诱导治疗第8天外周血MRD和第29天骨髓MRD资料完整的359例B-ALL患儿的数据。采用Spearman相关分析法探讨第8天外周血MRD与同期骨髓细胞形态学的相关性。采用Kaplan-Meier曲线分析第8天外周血MRD与无事件生存(EFS)的关系, 并分析第8天外周血MRD联合第29天骨髓MRD与EFS率的关系。采用Cox回归分析探讨B-ALL患儿预后的危险因素。
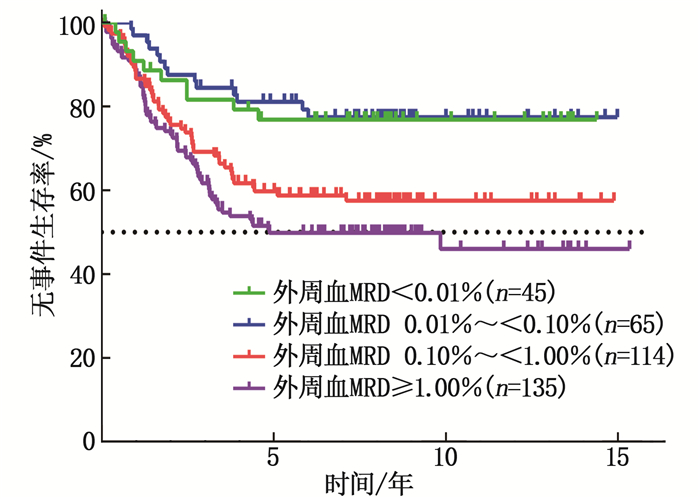
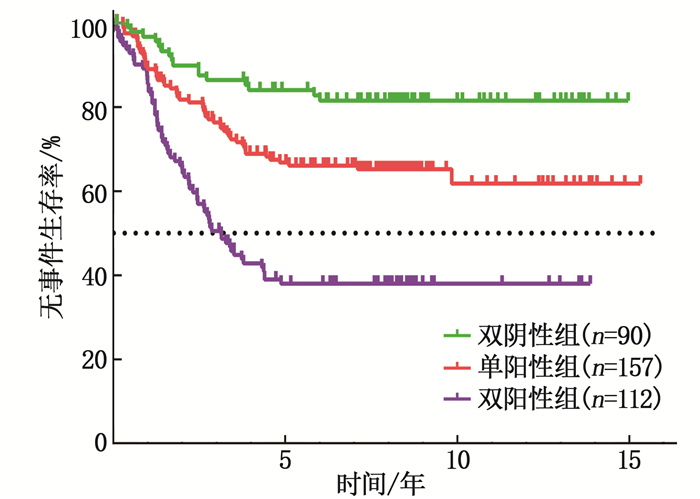
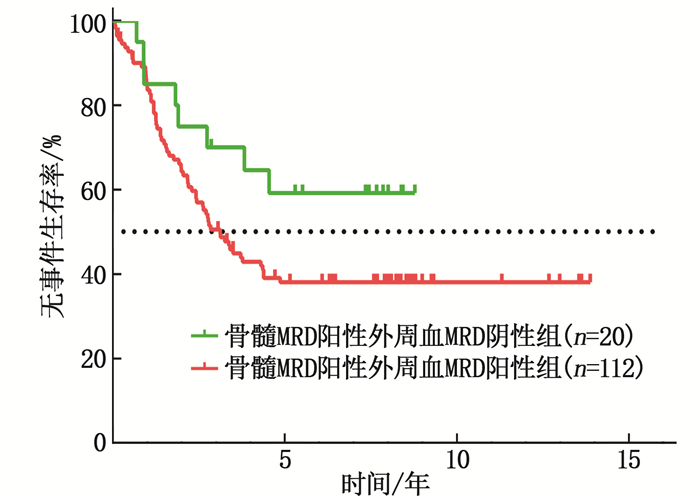
结果Spearman相关分析显示,第8天外周血MRD与同期骨髓原始细胞占比呈正相关(r=0.620, P < 0.001)。生存曲线显示,第8天外周血MRD < 0.01%、0.01%~ < 0.10%、0.10%~ < 1.00%、≥1.00%患儿的5年EFS率比较,差异有统计学意义(P < 0.001)。第8天外周血MRD与第29天骨髓MRD检测结果双阴性者预后最佳,单阳性者次之,双阳性者预后最差,差异有统计学意义(P < 0.001)。第29天骨髓MRD阴性患儿中,第8天外周血MRD阴性者的5年EFS率高于第8天外周血MRD阳性者,差异有统计学意义(P=0.009)。Cox回归分析显示,第8天外周血MRD≥0.10%(HR=1.967, 95%CI为1.234~3.134, P=0.004)、第29天骨髓MRD≥0.01%(HR=2.076, 95%CI为1.423~3.027, P < 0.001)均为B-ALL患儿EFS的独立危险因素。
结论诱导治疗第8天外周血MRD在儿童B-ALL预后评估中具有重要的临床意义,可作为第29天骨髓MRD的强有力补充。
Abstract:ObjectiveTo analyze clinical significance of peripheral blood minimal residual disease (MRD) detection at the eighth day of induction therapy in evaluating prognosis of children with B-cell acute lymphoblastic leukemia (B-ALL) based on the TARGET database.
MethodsData of 359 B-ALL children with peripheral blood MRD at the eighth day of induction therapy and bone marrow MRD at 29th day of induction therapy from year 2000 to 2010 were downloaded from TARGET database. Spearman correlation analysis was used to explore the association between peripheral blood MRD at the eighth day and morphology of bone marrow cells in the same period. Kaplan-Meier curve was used to analyze the relationship between peripheral blood MRD at the eighth day and event free survival (EFS), and further analyze the relationship of combined detection of peripheral blood MRD at the eighth day and bone marrow MRD at 29th day with EFS. Cox regression model was used to analyze the risk factors for prognosis in B-ALL children.
ResultsSpearman correlation analysis showed that the level of peripheral blood MRD at the eighth day was positively correlated with the proportion of bone marrow blasts at day 8 (r=0.620, P < 0.001). Survival analysis showed that there were significant differences in 5-year EFS rates of MRD < 0.01%, 0.01% to 0.10%, 0.10% to 1.00% and ≥ 1.00% in peripheral blood at the eighth day(P < 0.001). Double-negative patients with peripheral blood MRD at the 8th day and bone marrow MRD at the 29th day had the best prognosis, followed by single-positive patients, and double-positive patients had the worst prognosis, the differences were statistically significant (P < 0.001). The combined MRD at both time points showed that the prognosis was best in the double-negative group, followed by the single-positive group and worst in the double-positive group (P < 0.001). In children with negative bone marrow MRD at day 29, the 5-year EFS rate of children negative for MRD in peripheral blood at the eighth day was significantly higher than those positive for MRD in peripheral blood at the eighth day(P=0.009). Cox regression analysis showed that MRD ≥ 0.10% in peripheral blood on day 8(HR=1.967; 95%CI, 1.234 to 3.134; P=0.004), MRD ≥ 0.01% in bone marrow on day 29 (HR=2.076; 95%CI, 1.423 to 3.027; P < 0.001) were independent risk factors for EFS in B-ALL children.
ConclusionPeripheral blood MRD at day 8 of induction therapy has important clinical significance in prognosis assessment in children with B-ALL, and can be used as a strong supplement for the prognosis assessment of B-ALL children with bone marrow MRD at day 29.
-
-
表 1 359例B-ALL患儿的临床特征分析
特征 分类 [n(%)] 性别 男 219(61.0) 女 140(39.0) 年龄 < 10岁 176(49.0) ≥10岁 183(51.0) 白细胞 < 50×109/L 219(61.0) ≥50×109/L 140(39.0) TCF3-PBX1基因 阴性 321(89.4) 阳性 38(10.6) ETV6-RUNX1基因 阴性 324(90.3) 阳性 35(9.7) 4号和10号染色体三倍体 阴性 324(90.3) 阳性 35(9.7) MLL基因重排 阴性 337(93.9) 阳性 22(6.1) BCR-ABL1基因 阴性 353(98.3) 阳性 6(1.7) DNA指数 < q1.16 308(85.8) ≥1.16 51(14.2) 第8天骨髓原始细胞占比 < 20% 219(61.0) ≥20% 140(39.0) 第29天骨髓原始细胞占比 < 5% 349(97.2) ≥5% 10(2.8) 第8天外周血MRD < 0.01% 45(12.5) 0.01%~ < 0.10% 65(18.1) 0.10%~ < 1.00% 114(31.8) ≥1.00% 135(37.6) 第29天骨髓MRD < 0.01% 227(63.2) 0.01%~ < 0.10% 47(13.1) 0.10%~ < 1.00% 54(15.0) ≥1.00% 31(8.6) MRD: 微小残留病。 表 2 B-ALL患儿EFS的单因素和多因素Cox回归分析
变量 单因素分析 多因素分析 HR 95%CI P HR 95%CI P 年龄 1.205 0.859~1.688 0.280 — — — 白细胞 1.466 1.047~2.053 0.026 1.287 0.914~1.813 0.149 DNA指数 0.330 0.162~0.675 0.002 0.250 0.087~0.716 0.010 ETV6-RUNX1基因 0.412 0.192~0.881 0.022 0.540 0.250~1.170 0.118 4号和10号染色体三倍体 0.427 0.200~0.914 0.028 1.541 0.501~4.736 0.450 MLL基因重排 1.560 0.841~2.894 0.159 — — — TCF3-PBX1基因 1.253 0.744~2.112 0.396 — — — BCR-ABL1基因 1.622 0.516~5.095 0.407 — — — 第8天骨髓原始细胞占比 1.866 1.332~2.613 < 0.001 1.070 0.731~1.567 0.726 第29天骨髓原始细胞占比 4.404 2.236~8.676 < 0.001 2.636 1.309~5.307 0.007 第8天外周血MRD 2.502 1.609~3.890 < 0.001 1.967 1.234~3.134 0.004 第29天骨髓MRD 2.720 1.937~3.820 < 0.001 2.076 1.423~3.027 < 0.001 MRD: 微小残留病。 -
[1] PUI C H, YANG J J, HUNGER S P, et al. Childhood acute lymphoblastic leukemia: progress through collaboration[J]. J Clin Oncol, 2015, 33(27): 2938-2948. doi: 10.1200/JCO.2014.59.1636
[2] 冯静, 陈晓娟, 刘晓明, 等. 多参数流式细胞术检测的微小残留病与儿童急性B淋巴细胞白血病预后的相关性研究[J]. 中华血液学杂志, 2019, 40(8): 678-680. [3] JABBOUR E, GÖKBUGET N, ADVANI A, et al. Impact of minimal residual disease status in patients with relapsed/refractory acute lymphoblastic leukemia treated with inotuzumab ozogamicin in the phase Ⅲ INO-VATE trial[J]. Leuk Res, 2020, 88: 106283. doi: 10.1016/j.leukres.2019.106283
[4] 丁超, 单建芝, 吕娅, 等. 急性淋巴细胞白血病微小残留病检测的方法、标本选择、临床意义研究进展[J]. 山东医药, 2019, 59(6): 103-106. doi: 10.3969/j.issn.1002-266X.2019.06.029 [5] BROWN P, INABA H, ANNESLEY C, et al. Pediatric acute lymphoblastic leukemia, version 2.2020, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2020, 18(1): 81-112. doi: 10.6004/jnccn.2020.0001
[6] 吕敏, 田国祥, 郭晓娟, 等. TARGET数据库的介绍及数据提取[J]. 中国循证心血管医学杂志, 2019, 11(4): 387-390. doi: 10.3969/j.issn.1674-4055.2019.04.02 [7] 中华医学会儿科学分会血液学组, 《中华儿科杂志》编辑委员会. 儿童急性淋巴细胞白血病诊疗建议(第四次修订)[J]. 中华儿科杂志, 2014, 52(9): 641-644. doi: 10.3760/cma.j.issn.0578-1310.2014.09.001 [8] 中华医学会儿科学分会血液学组, 中华儿科杂志编辑委员会. 儿童急性淋巴细胞白血病诊疗建议(第三次修订草案)[J]. 中华儿科杂志, 2006, 44(5): 392-395. doi: 10.3760/j.issn:0578-1310.2006.05.023 [9] BOROWITZ M J, PULLEN D J, SHUSTER J J, et al. Minimal residual disease detection in childhood precursor-B-cell acute lymphoblastic leukemia: relation to other risk factors. A Children's Oncology Group study[J]. Leukemia, 2003, 17(8): 1566-1572. doi: 10.1038/sj.leu.2403001
[10] BOROWITZ M J, DEVIDAS M, HUNGER S P, et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia and its relationship to other prognostic factors: a Children's Oncology Group study[J]. Blood, 2008, 111(12): 5477-5485. doi: 10.1182/blood-2008-01-132837
[11] MAO R, HU S X, ZHANG Y C, et al. Prognostic nomogram for childhood acute lymphoblastic leukemia: a comprehensive analysis of 673 patients[J]. Front Oncol, 2020, 10: 1673. doi: 10.3389/fonc.2020.01673
[12] VAN DER VELDEN V H J, JACOBS D C H, WIJKHUIJS A J M, et al. Minimal residual disease levels in bone marrow and peripheral blood are comparable in children with T cell acute lymphoblastic leukemia (ALL), but not in precursor-B-ALL[J]. Leukemia, 2002, 16(8): 1432-1436. doi: 10.1038/sj.leu.2402636
[13] COUSTAN-SMITH E, SANCHO J, HANCOCK M L, et al. Use of peripheral blood instead of bone marrow to monitor residual disease in children with acute lymphoblastic leukemia[J]. Blood, 2002, 100(7): 2399-2402. doi: 10.1182/blood-2002-04-1130
[14] 葛丽卫, 王笑颜. 流式细胞术用于白血病外周血细胞检测对急性白血病复发判断的意义[J]. 检验医学, 2018, 33(3): 239-241. doi: 10.3969/j.issn.1673-8640.2018.03.012 [15] 程丽萍, 张莉. 家长认知行为干预在提高白血病患儿治疗依从性中的应用研究[J]. 实用临床医药杂志, 2017, 21(16): 214-216. doi: 10.7619/jcmp.201716076 [16] WOOD B, WU D, CROSSLEY B, et al. Measurable residual disease detection by high-throughput sequencing improves risk stratification for pediatric B-ALL[J]. Blood, 2018, 131(12): 1350-1359. doi: 10.1182/blood-2017-09-806521
[17] MUFFLY L, SUNDARAM V, CHEN C, et al. Concordance of peripheral blood and bone marrow measurable residual disease in adult acute lymphoblastic leukemia[J]. Blood Adv, 2021, 5(16): 3147-3151. doi: 10.1182/bloodadvances.2021004234
[18] BARTRAM J, WRIGHT G, ADAMS S, et al. High-throughput sequencing of peripheral blood for minimal residual disease monitoring in childhood precursor B-cell acute lymphoblastic leukemia: a prospective feasibility study[J]. Pediatr Blood Cancer, 2022, 69(3): e29513.
[19] 李红, 邵静波, 朱嘉莳, 等. 儿童急性淋巴细胞白血病早期治疗反应对预后的预测价值[J]. 临床儿科杂志, 2021, 39(8): 600-604. doi: 10.3969/j.issn.1000-3606.2021.08.010 [20] 安粉艳, 张淑红, 孔令军, 等. 微量残留病在儿童B系急性淋巴细胞白血病危险分层及预后中的临床意义[J]. 中国实验血液学杂志, 2017, 25(3): 729-735. [21] PIETERS R, DE GROOT-KRUSEMAN H, VAN DER VELDEN V, et al. Successful therapy reduction and intensification for childhood acute lymphoblastic leukemia based on minimal residual disease monitoring: study ALL10 from the Dutch childhood oncology group[J]. J Clin Oncol, 2016, 34(22): 2591-2601. doi: 10.1200/JCO.2015.64.6364
[22] 薛玉娟, 陆爱东, 王毓, 等. 微小残留病在儿童急性B淋巴细胞白血病预后中的意义[J]. 临床儿科杂志, 2021, 39(5): 321-326. doi: 10.3969/j.issn.1000-3606.2021.05.001 [23] O'CONNOR D, MOORMAN A V, WADE R, et al. Use of minimal residual disease assessment to redefine induction failure in pediatric acute lymphoblastic leukemia[J]. J Clin Oncol, 2017, 35(6): 660-667. doi: 10.1200/JCO.2016.69.6278
-
期刊类型引用(10)
1. 黄艳,梁玉美,冯燕妮,杨松媚. 外周血受体相互作用蛋白激酶3、混合系列蛋白激酶样结构域水平与新生儿坏死性小肠结肠炎病情严重程度的关系. 实用临床医药杂志. 2024(01): 62-67 .  本站查看
本站查看
2. 庄丽霞,张结,陈培鑫. 血清转化生长因子-β1、肠碱性磷酸酶诊断重症新生儿坏死性小肠结肠炎的应用价值研究. 实用临床医药杂志. 2023(19): 67-70 .  本站查看
本站查看
3. 梁元豪,郭红梅,梁燕勇,王霞. 超声和X线片检查运用于新生儿坏死性小肠结肠炎的诊断效果观察. 中外医学研究. 2021(05): 78-80 .  百度学术
百度学术
4. 温晓敏,张爱明,叶明阳,王文翔. 尿I-FABP联合CBG诊断新生儿坏死性小肠结肠炎的价值分析. 中国实验诊断学. 2021(06): 853-857 .  百度学术
百度学术
5. 张宁,杨秀玲. X线评分量表联合腹部超声可较好识别新生儿坏死性小肠结肠炎:89例前瞻性研究. 分子影像学杂志. 2021(03): 526-530 .  百度学术
百度学术
6. 苏嘉鸿,钟陈,胡小华. 新生儿坏死性小肠结肠炎和先天性巨结肠肠穿孔的鉴别诊断和治疗分析. 世界复合医学. 2021(10): 115-118 .  百度学术
百度学术
7. 余凤,蒋双兰,毛伟豪. 新生儿坏死性小肠结肠炎的早期诊断及效果观察. 现代医用影像学. 2020(01): 137-138 .  百度学术
百度学术
8. 黄文生,钟小明,罗开源,肖洪亮,郭荣华,黄毅,谢海燕. 钙卫蛋白结合直肠液渗透压在NEC诊断及病情监测中的应用研究. 中国现代医生. 2020(19): 14-16 .  百度学术
百度学术
9. 王晶,曾朝强,张福洲,陈世孝,母其文,尚彪,田鹏. 新生儿坏死性小肠结肠炎的X线诊断分析. 实用医学影像杂志. 2020(05): 456-458 .  百度学术
百度学术
10. 范文婷,廖伟. 新生儿坏死性小肠结肠炎发生的主要危险因素及手术时机对预后影响的回顾性分析. 川北医学院学报. 2019(06): 679-682 .  百度学术
百度学术
其他类型引用(2)




 下载:
下载:


 苏公网安备 32100302010246号
苏公网安备 32100302010246号
